Meta-Analysis J Dent . 2019 Mar;82:11-21.
doi: 10.1016/j.jdent.2018.12.014. Epub 2019 Jan 3.
Clinical efficacy of nano-hydroxyapatite in dentin hypersensitivity: A systematic review and meta-analysis
Cristiane de Melo Alencar 1 , Brennda Lucy Freitas de Paula 1 , Mariangela Ivette Guanipa Ortiz 1 , Marcela Baraúna Magno 2 , Cecy Martins Silva 3 , Lucianne Cople Maia 2
Affiliations
-
1 School of Dentistry, Federal University of Para, Belém, PA, Brazil.
-
2 School of Dentistry, Federal University of Rio de Janeiro, Rio de Janeiro, RJ, Brazil.
-
3 School of Dentistry, Federal University of Para, Belém, PA, Brazil. Electronic address: cecymsilva@gmail.com.
Abstract
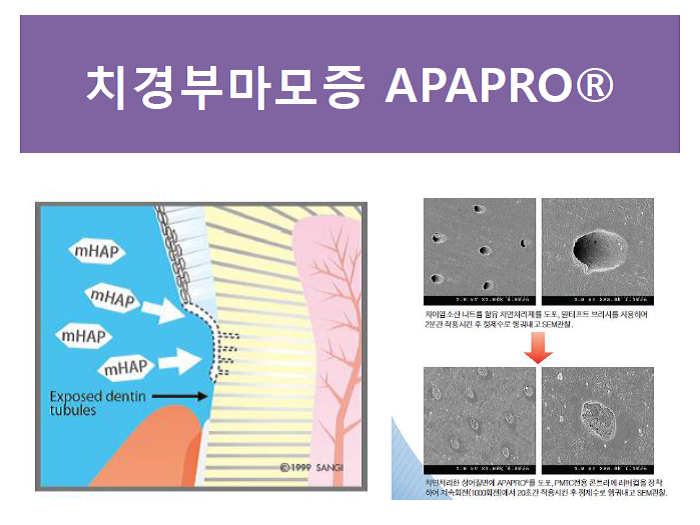
Objectives: To evaluate the desensitizing effect of nano-hydroxyapatite (n-HAP) on dentine hypersensitivity (DH).
Sources: Seven electronic databases were searched on April 27, 2018.
Study selection: Randomized clinical trials (RCTs) were included based on the PICO strategy: Participants - Humans with DH; Intervention - n-HAP-containing desensitizing; Comparison -n-HAP-free treatments or placebo/negative control; and Outcomes - relief of DH. The risk of bias was classified by the Cochrane guidelines. Five meta-analyses were performed to evaluate the efficacy of n-HAP with regard to pain assessment stimuli (primary outcome); comparison of n-HAP with other treatments or placebo/negative control, and effectiveness of at-home and in-office n-HAP use (secondary outcomes). The quality of the evidence was evaluated using the GRADE.
Data: Six RCTs with 4 weeks of follow-up were included in the meta-analysis. For the primary outcome, n-HAP showed a better desensitizing effect for evaporative stimuli (SMD -1.09 [-1.24, -0.94], p < 0.00001) and tactile stimuli (SMD -0.93 [-1.42, -0.43]) than other treatments (p = 0.0002). However, there was no difference between n-HAP and other treatments for the cold stimuli (SMD -0.17 [-0.81, 0.48], p = 0.61). In an overall analysis, n-HAP-containing treatment showing the most significant desensitizing effect (SMD -0.93 [-1.19, -0.68], p < 0.00001) with a high quality of evidence for pooled results. In the secondary outcomes, n-HAP showed the best effect in the overall analysis (p < 0.05) with moderate quality evidence.
Conclusions: The n-HAP-containing treatment showed better clinical performance than other treatments for DH relief. However, long-term follow-up RCTs are required in the future before definitive recommendations can be made.
Clinical significance: Dentin hypersensitivity is a common global condition and its multifactorial etiology has led to the development of several treatments. The n-HAP-containing treatment showed greater DH relief when compared to other desensitizing agents, placebo or negative control.
Keywords: Clinical trials; Dentin hypersensitivity; Desensitizing agents; Meta-analysis.

'충치예방(치아재광화)' 카테고리의 다른 글
| 우리가 알아야 할 치면 손상 위험들: 플라그, 치면 스크래치, 탈회, 치근면노출, 치면착색 (0) | 2020.11.18 |
|---|---|
| 아파프로 나노케어 예방 세미나 (0) | 2020.11.11 |
| '아파프로 나노케어' 신개념 치과 예방세미나 (0) | 2020.10.27 |
| 전문가를 위한 나노 하이드록시아파타이트 치아재광화 페이스트 '에나멜 리페어' (0) | 2020.10.27 |
| 치아교정시 구강관리(치아,잇몸)엔 아파프로! (0) | 2020.09.24 |



